If you’ve ever watched a zombie movie and thought, “Well, at least it’s not real,” I’ve got bad news: flesh-eating bacteria is about as close as nature gets to an actual zombie attack. Officially called necrotizing fasciitis, this is one of those rare conditions that can turn a tiny paper cut into a full-on medical emergency in just hours. The name sounds over the top, but this is one case where the hype is 100% justified.
Flesh-eating bacteria vs. common skin infections isn’t just a medical trivia question—it’s something you really do want to be able to tell apart. Because while a pimple or scraped knee might just need some soap and a bandage, necrotizing fasciitis can progress faster than your phone battery drops at 1%.
In simple terms: Flesh-eating bacteria can destroy skin, muscle, and tissue in hours, while most common skin infections are slow-moving and far less aggressive.
What Is Necrotizing Fasciitis, Really?
Let’s start with the basics before we spiral into panic Googling.
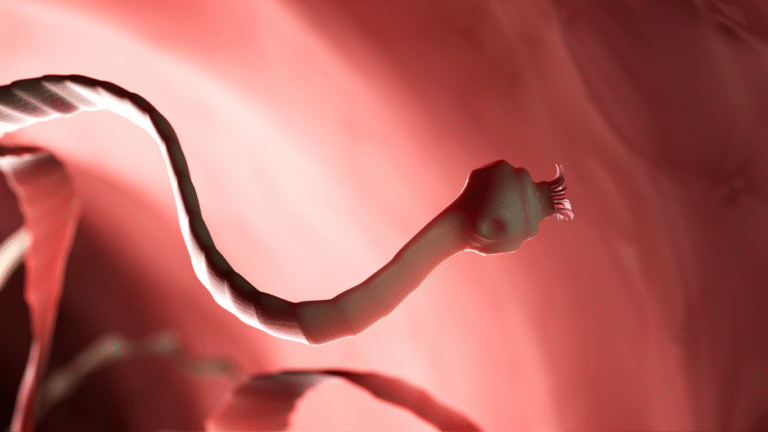
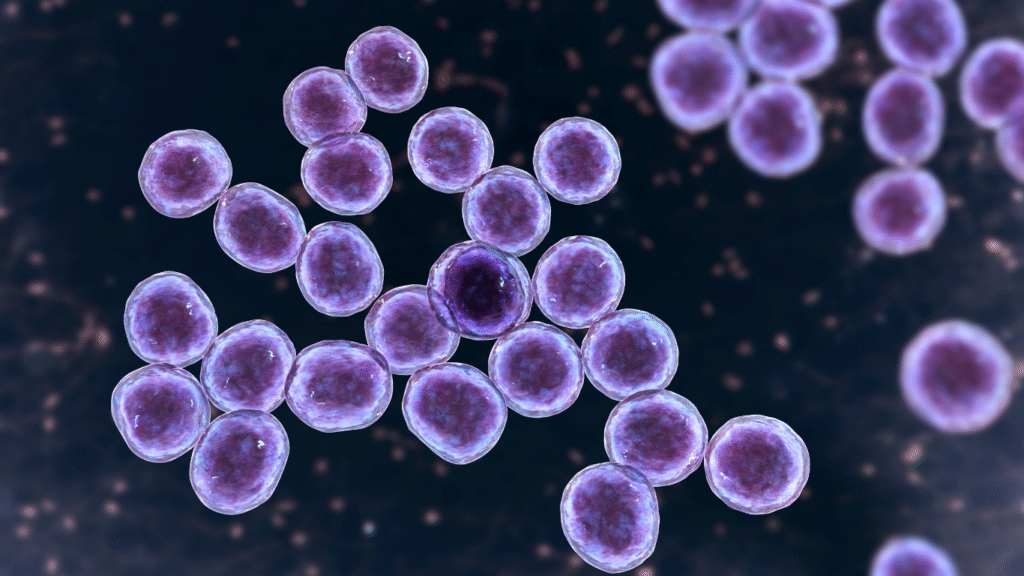
Necrotizing fasciitis is a severe infection that usually starts when bacteria—most often Group A Streptococcus—slip past your skin’s defenses. This can happen through even the smallest break in the skin: a shaving nick, a bug bite, a blister from your new sneakers. Once inside, the bacteria spread like a bad rumor, releasing toxins that literally kill the surrounding tissue.
The scary part? It doesn’t just stay in one place. This infection can travel under the skin along the connective tissue (called the fascia) at alarming speed, leaving the surface looking deceptively normal at first. Meanwhile, below the skin, the bacteria are doing damage you can’t see.
Common skin infections—like impetigo, cellulitis, or folliculitis—are typically localized and slow to progress. They might cause redness, swelling, and discomfort, but they don’t usually melt through tissue like hot butter.
Who’s Most at Risk?
Necrotizing fasciitis doesn’t discriminate, but it does have some favorite targets. People with weakened immune systems, chronic illnesses like diabetes, cancer, or liver disease are more vulnerable. So are those with recent surgery or wounds.
That said, healthy individuals aren’t off the hook. Cases have occurred after swimming in warm coastal waters, fishing, or even after a minor scrape in a garden. In rare cases, a routine activity like shaving your legs or trimming your toenails can be the starting point.
So, no—this isn’t just an “older people” or “hospital-acquired” problem. It’s a “humans with skin” problem.
Symptoms You Should Never Ignore
Here’s where things get tricky. Early necrotizing fasciitis symptoms can be sneaky. They often mimic mild skin infections or even the flu. That’s why knowing the red flags can be life-saving.
Watch for:
- Intense pain that feels way worse than the wound looks. If you’re clutching your arm like you’ve been hit by a truck but the cut is the size of a pencil eraser, that’s a red flag.
- Rapid swelling around the injury site.
- Skin discoloration, starting with redness and quickly turning to purple or gray patches.
- Blisters or fluid-filled bumps near the wound.
- Fever, chills, and fatigue that come on fast.
By contrast, common skin infections usually start with mild redness and tenderness, and they worsen gradually over several days—not hours.
How Doctors Tell the Difference
If you head to the ER, doctors don’t just rely on “gut feeling” (though experienced physicians can sometimes spot it instantly). They may:
- Ask about timing — Necrotizing fasciitis progresses frighteningly fast.
- Check pain vs. appearance — Severe pain with minimal surface changes is suspicious.
- Run blood tests — High white blood cell counts and other markers can signal severe infection.
- Use imaging — CT scans or MRIs can show tissue damage below the skin.
Bottom line: if you think you might have flesh-eating bacteria, don’t wait for it to “get worse.” By the time it does, you could be in serious trouble.
Treatment: The Race Against Time
When it comes to necrotizing fasciitis, doctors don’t play the “let’s wait and see” game. Treatment usually includes:
- Immediate high-dose antibiotics through an IV.
- Emergency surgery to remove dead tissue and stop the spread.
- Supportive care like fluids, pain management, and sometimes oxygen therapy.
For common skin infections, treatments might just be topical creams, oral antibiotics, or even home care. That’s the big difference: one can be handled with a pharmacy run, the other needs an OR and a medical team working overtime.
Prevention: Keeping the Monster Out
You can’t 100% prevent necrotizing fasciitis, but you can stack the odds in your favor:
- Clean even small wounds with soap and water.
- Keep cuts covered until healed.
- Avoid swimming in natural bodies of water with open wounds.
- Treat skin infections promptly—don’t “wait it out.”
A regular skin infection might give you a few days’ grace period. Flesh-eating bacteria will not.
Quick Facts Worth Sharing
- Flesh-eating bacteria can destroy tissue in less than 24 hours.
- Common skin infections are usually slow, localized, and easily treated.
- Warm, brackish water can harbor dangerous bacteria—think twice before wading in with an open cut.
Why It Matters to You
Knowing the difference between flesh-eating bacteria and a common skin infection isn’t just about avoiding medical bills—it’s about protecting your life. The earlier necrotizing fasciitis is caught, the higher the chances of recovery without severe complications.
Your skin is your first defense barrier. Treat it with the same respect you’d give your phone screen—because once it’s damaged, things can escalate quickly.
Recap: Key Takeaways
- Necrotizing fasciitis = fast, deadly, needs urgent treatment.
- Common skin infections = slow, localized, often mild.
- Early recognition can save your life.
- Prevention is simple but essential.
Sources:
- Centers for Disease Control and Prevention (CDC) – Necrotizing Fasciitis Overview: https://www.cdc.gov/groupastrep/diseases-public/necrotizing-fasciitis.html
- World Health Organization (WHO) – Antimicrobial Resistance and Necrotizing Fasciitis: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
- National Institutes of Health (NIH) – Necrotizing Soft Tissue Infections Review: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5653360/