Discover how antibiotic resistance is growing, why it’s a global threat to health and medicine, and what steps you can take to make a difference.
What if your deepest worry is that one day even a simple infection could become untreatable, potentially leading to severe illness or worse? You just want to understand how we ended up in this precarious position and what concrete actions you can take to protect yourself and future generations. If you keep reading, you’ll grasp exactly how antibiotic resistance spreads . , . and how your daily choices critically matter to keeping modern medicine alive.
Why understanding How Antibiotic Resistance Happens . , . and Why It’s Everyone’s Problem matters more than many people realize. This isn’t some abstract scientific concept confined to laboratories. It’s a looming global crisis actively shaping our future health, threatening the safety of routine medical procedures, and jeopardizing even the most basic medical care we currently take for granted.
However, some might dismiss antibiotic resistance as merely a hospital issue, or a problem that will simply be solved with the invention of new pharmaceuticals. This perspective, unfortunately, misses the bigger picture. On the other hand, medical experts and scientists warn that resistance flows unchecked through farms, clinics, and households, affecting every single person. And simply inventing new drugs, while important, isn’t nearly enough to combat this rapidly evolving threat.
1. How Resistance Actually Happens
Antibiotic resistance fundamentally starts with basic bacterial biology. However, human habits and widespread practices dramatically amplify its spread.
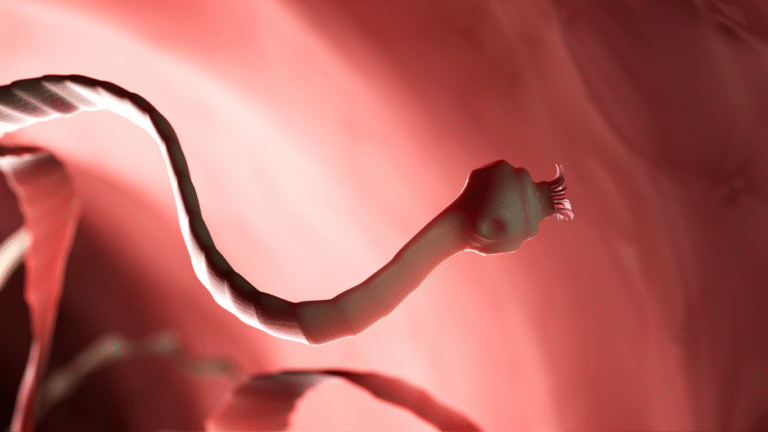
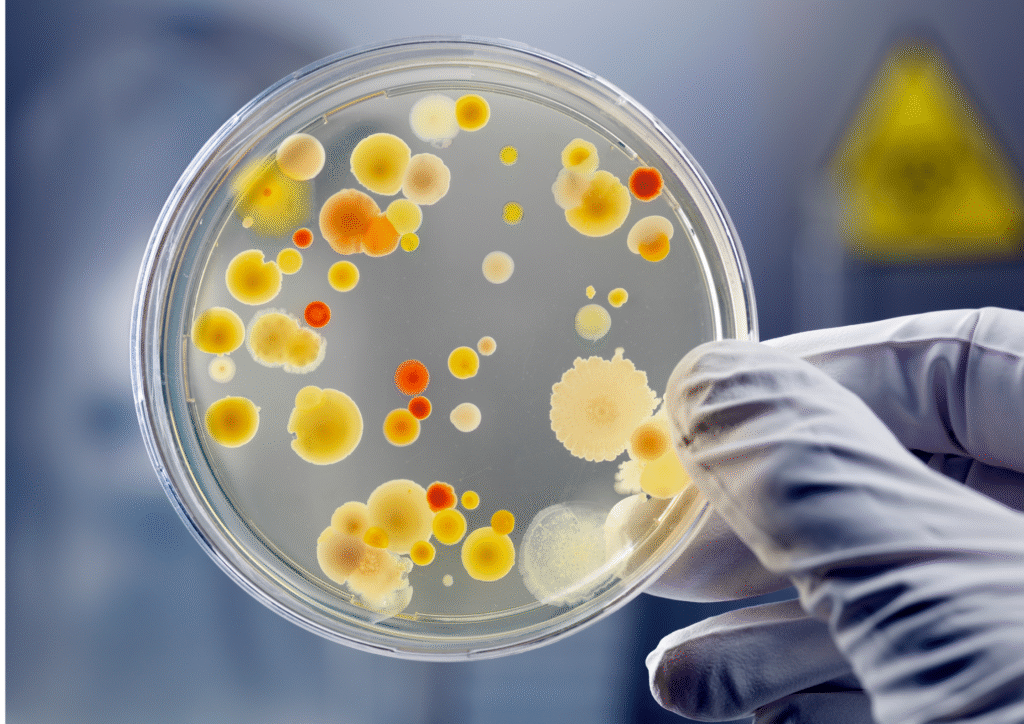
Bacteria, like all living organisms, naturally mutate. Among these mutations, some might randomly develop genes that provide resistance to antibiotics. When antibiotics are used, these resistant bacteria survive, while non-resistant ones are killed off. This creates a powerful selective pressure, allowing the resistant strains to multiply and dominate. [1, 2] What’s more concerning is that these resistance genes can then spread horizontally between bacteria, even to different species, through processes like plasmid transfer. [3, 4] The widespread overuse and misuse of antibiotics in both human medicine and livestock fast-tracks this dangerous evolutionary process, accelerating the emergence of resistant strains. [1, 5] As a result, once-rare “superbugs” are now common in many environments . , . and are becoming incredibly difficult, or impossible, to treat with existing medications.
2. Numbers We Can’t Ignore
The statistics on antibiotic resistance are stark and sobering, painting a clear picture of a growing global health burden.
Globally, in 2019 alone, at least 1.27 million deaths were directly attributed to antimicrobial-resistant infections, with nearly 5 million more deaths linked to them. [6] In the United States, the Centers for Disease Control and Prevention (CDC) estimates that antibiotic-resistant bacteria cause 2.8 million infections each year, tragically resulting in over 35,000 deaths. [6, 7] Furthermore, during the COVID-19 pandemic, resistant infections saw a concerning 20% increase. This surge was primarily driven by the overprescription of antibiotics for viral infections (for which they are ineffective) and by weakened healthcare systems. [8] On a more positive note, there have been some gains. For instance, hospital-acquired MRSA (methicillin-resistant Staphylococcus aureus) rates dropped by 17% between 2005 and 2012 in the U.S. due to improved infection control and hygiene practices. [9] This demonstrates that collective action can indeed make a difference.
3. It’s Everyone’s Problem . . . Not Just Hospitals
The reach of antibiotic resistance extends far beyond hospital walls, infiltrating our daily lives from multiple, interconnected areas.
The widespread use of antibiotics in livestock, particularly to promote growth or prevent illness in crowded conditions, drives resistant bacteria into the food chain and subsequently into our water systems. [5] Beyond agriculture, waste from pharmaceutical factories, farms, and inadequately treated wastewater systems actively contributes to the environmental spread of resistance genes across communities. [10] And, unfortunately, the misuse of antibiotics in human health, such as demanding them for viral illnesses like colds or the flu (against which antibiotics are powerless), directly adds fuel to this evolving crisis. [11, 12] This explainer on How Antibiotic Resistance Happens . , . and Why It’s Everyone’s Problem clearly shows why it urgently demands action from individuals, farmers, doctors, and policymakers alike.
4. Why We Can’t Just Keep Creating New Drugs
Developing new antibiotics is undoubtedly vital. However, the pharmaceutical pipeline for truly novel drugs is rapidly drying up, presenting a significant challenge.
Broad-spectrum antibiotics, designed to target a wide range of bacteria, are incredibly expensive and time-consuming to develop. Despite their critical importance, they are often underused after approval to preserve their effectiveness, making them less profitable for pharmaceutical companies. [13] Initiatives like the U.S. Pasteur Act aim to offer critical funding and market incentives for novel antibiotic development, yet global access to these new drugs remains uneven. [13] Crucially, without stringent reinforcement through responsible use, bacteria will inevitably evolve resistance even against brand-new drugs. As a result, we need smarter, more strategic use of the antibiotics we currently have, rather than simply relying on an endless supply of new ones.
5. What Each of Us Can Do
Combating antibiotic resistance doesn’t require a scientific degree. There are crucial, impactful steps that each of us can take in our daily lives.
- Use antibiotics only when prescribed: Never self-medicate or share antibiotics with others. Take them only when a doctor has determined they are necessary for a bacterial infection. [11, 14]
- Finish the full course: Complete the entire prescribed course of antibiotics, even if you start feeling better quickly. Stopping early can leave stronger, more resistant bacteria behind. [11, 12]
- Say no to antibiotics for viruses: Understand that antibiotics are ineffective against viral infections like colds, flu, or most sore throats. Do not pressure your doctor for antibiotics in these cases. [11, 12]
- Support antibiotic-free farming: Make conscious choices to buy meat and poultry from sources that raise animals without the routine use of antibiotics. This reduces pressure for resistance development in agriculture. [5]
- Stay updated on vaccines: Regular vaccinations protect you from common bacterial and viral infections, thereby reducing your need for antibiotics. [15]
- Practice good hygiene: Simple, consistent practices like thorough handwashing remain your most effective defense against the spread of germs, reducing the overall need for antibiotics. [15]
Empathy Before Critique
It’s important to acknowledge the complex pressures faced by those on the front lines of antibiotic use. Many doctors and farmers feel immense pressure to prescribe or medicate animals for quick results.
Farmers often feel they need antibiotics to keep livestock healthy and alive, especially under crowded conditions common in modern agriculture. Doctors, too, may feel rushed or pressured by patient expectations to prescribe antibiotics, even when they know it’s not the best course of action for a viral illness. [16] However, collective efforts, such as antibiotic stewardship programs in healthcare and agriculture, are proving that these systems can indeed shift when given proper support, education, and resources. [17] This collaborative approach is vital for long-term success.
Dark Humor Moment
I once lied to my doctor about needing antibiotics for a cold . , . then later Googled “side effects of not finishing your antibiotic dose.” Spoiler alert: it’s a horror story starring your own immune system becoming a hotbed for superbugs.
Why This Matters to You
Antibiotic resistance isn’t just a distant problem. It jeopardizes every aspect of modern medicine and daily life.
- It makes routine surgeries and childbirth riskier: Common procedures become life-threatening when post-operative infections can’t be treated.
- It may lead us back to a pre-antibiotic era: A time when minor cuts, strep throat, or even childbirth could be fatal due, to untreatable infections. [13]
- It burdens global health systems: Resistant infections are more expensive to treat, requiring longer hospital stays and more complex, costly drugs. This burden disproportionately affects low-income countries. [1, 5]
Conclusion & Your Next Step
Antibiotic resistance isn’t someone else’s problem. It’s a very real and present future health crisis that we can still mitigate through collective, conscious everyday choices. Your actions, no matter how small, contribute to the global effort.
Your Next Step: Commit to antibiotic stewardship today. Always ask your doctor questions about why an antibiotic is being prescribed. Choose meat from trusted sources that prioritize responsible antibiotic use. Wash your hands thoroughly and regularly. And encourage your friends and family to do the same. Because preserving the effectiveness of antibiotics means protecting our lives, our families, and our future. We all share this profound responsibility . , . and our collective actions now will echo for generations to come.
Sources
- World Health Organization (WHO). “Antibiotic resistance.” Updated November 17, 2021. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance
- Centers for Disease Control and Prevention (CDC). “How Antibiotic Resistance Happens.” Updated March 15, 2023. https://www.cdc.gov/drugresistance/about/how-resistance-happens.html
- Nature Reviews Microbiology. “Horizontal gene transfer and the global spread of antibiotic resistance.” Published May 2010. https://www.nature.com/articles/nrmicro2352
- PLoS Pathogens. “Mobile Genetic Elements and Antimicrobial Resistance.” Published July 25, 2019. https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1007817
- The Pew Charitable Trusts. “How Antibiotics Are Used in Food Animals.” Published April 26, 2016. https://www.pewtrusts.org/en/research-and-analysis/fact-sheets/2016/04/how-antibiotics-are-used-in-food-animals
- The Lancet. “Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis.” Published January 19, 2022. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)02724-0/fulltext
- Centers for Disease Control and Prevention (CDC). “Antibiotic Resistance Threats in the United States, 2019.” Published 2019. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf
- Centers for Disease Control and Prevention (CDC). “COVID-19 U.S. Impact on Antimicrobial Resistance.” Updated July 13, 2021. https://www.cdc.gov/drugresistance/covid19.html
- The New England Journal of Medicine. “Decline in Hospital-Acquired MRSA Infections.” Published September 11, 2014. https://www.nejm.org/doi/full/10.1056/NEJMoa1311394
- Nature Microbiology. “Antibiotic resistance genes in the environment.” Published February 2017. https://www.nature.com/articles/nmicrobiol.2016.241
- Centers for Disease Control and Prevention (CDC). “Antibiotic Prescribing and Use.” Updated November 2, 2023. https://www.cdc.gov/antibiotic-use/core-elements/patients.html
- World Health Organization (WHO). “Five facts about antibiotic resistance.” Accessed July 17, 2025. https://www.who.int/campaigns/world-antibiotic-awareness-week/2021/five-facts-about-antibiotic-resistance
- The Pew Charitable Trusts. “The Antibiotic Pipeline: A Snapshot of the Global Clinical Pipeline of New Antibiotics and Other Treatments for Bacterial Infections.” Published March 2024. https://www.pewtrusts.org/-/media/assets/2024/03/antibiotic-pipeline-report_march-2024.pdf
- World Health Organization (WHO). “World Antimicrobial Awareness Week 2023.” Accessed July 17, 2025. https://www.who.int/campaigns/world-antimicrobial-awareness-week
- Centers for Disease Control and Prevention (CDC). “Prevention Strategies for Antibiotic Resistance.” Updated November 2, 2023. https://www.cdc.gov/drugresistance/pdf/threats-report/prevention-strategies.pdf
- NPR. “Doctors Under Pressure: How Patient Demands Fuel Antibiotic Overuse.” Published December 1, 2014. https://www.npr.org/sections/health-shots/2014/12/01/367673550/doctors-under-pressure-how-patient-demands-fuel-antibiotic-overuse
- Centers for Disease Control and Prevention (CDC). “Antibiotic Stewardship.” Updated July 18, 2024. https://www.cdc.gov/antibiotic-use/antibiotic-stewardship.html