Uncover the hidden truths about acne-causing bacteria and why common skincare products might make your breakouts worse, not better.
What if your deepest wish is clear, confident skin, but every new cream, cleanser, or spot treatment you try just seems to make things worse? You’re caught in a cycle of frustration, unsure what to trust. If you keep reading, you’ll understand the real, nuanced role bacteria play in acne, and why some popular products actually backfire, leading to more breakouts instead of clear skin.
Why knowing How Bacteria on Your Skin Impacts Acne matters more than you think. Because acne isn’t just a surface issue or a matter of “cleanliness.” It’s deeply connected to a hidden, complex world of skin microbes. Getting this bacterial balance right changes everything for your complexion and confidence.
However, many traditional skincare routines focus solely on aggressively killing bacteria, operating under the assumption that all bacteria on your skin are inherently “bad.” On the other hand, cutting-edge research now shows the mix and specific strains of bacteria matter far more than their sheer volume. Treating everything like the enemy can severely disrupt your skin’s natural, protective balance, leading to unintended consequences.
How Bacteria Cause or Calm Acne
Our skin is a living ecosystem, teeming with millions of microscopic microbes. Most of these are harmless, and many actually play a crucial role in protecting us from external threats.
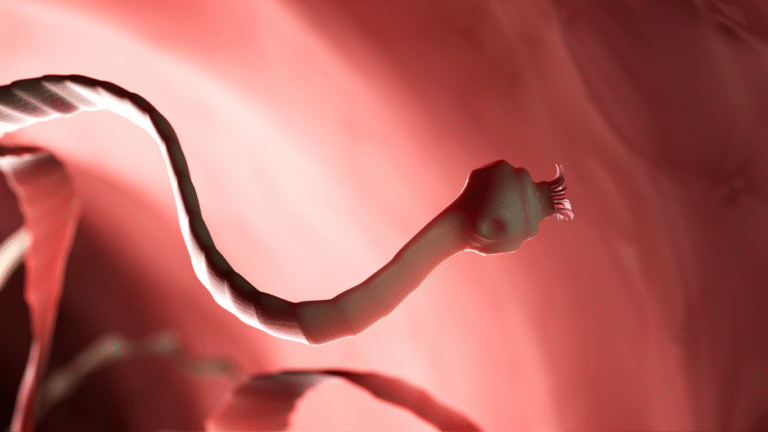
Cutibacterium acnes (formerly known as P. acnes) is the usual bacterial suspect commonly associated with acne. This bacterium thrives on the oil (sebum) in your pores. Once there, it produces inflammatory enzymes and sends immune signals into your pores, triggering the redness, swelling, and pus characteristic of acne lesions. [1, 2]
However, the surprising truth is that not all C. acnes strains are your enemies. Groundbreaking research from UCLA, led by Dr. Huiying Li, found that acne-prone skin often harbors specific, “virulent” strains of C. acnes. In contrast, clear, healthy skin tends to carry protective, beneficial variants of the same bacterium. [3, 4]
“Everybody has P. acnes, but it’s the bad strains that cause inflammation.” — Dr. Huiying Li, UCLA [4]
As a result, acne management isn’t simply about eliminating all bacteria from your skin. Instead, true, lasting improvement comes from restoring a healthy, balanced microbial ecosystem on your skin’s surface.
Product Pitfall #1: Harsh Cleansers & Over-Washing
Many individuals suffering from acne believe that scrubbing harder and washing more frequently will lead to clearer skin. This often feels intuitive: “If it’s dirty, clean it aggressively.”
But here’s the problem with this approach: Over-washing, especially with harsh cleansers, actively strips your skin of its natural, protective oils. This damages your crucial skin barrier, making it more vulnerable. Paradoxically, this stripping often triggers your skin to produce even more oil, exacerbating the problem. [5] As a result, irritation increases, the skin barrier breaks down, and opportunistic bacteria can penetrate deeper into pores, ultimately making acne much worse. On the other hand, a gentle, balanced cleansing routine helps keep your skin’s natural defenses intact, fostering a healthier environment for beneficial microbes.
Product Pitfall #2: Alcohol-Based Astringents & Spot Treatments
Products containing high concentrations of rubbing alcohol or aggressive formulations of benzoyl peroxide have long been traditional go-tos for acne spot treatments.
But contemporary research warns against their indiscriminate use: Alcohol, while providing a temporary sensation of “cleanliness,” severely strips essential skin oils and disrupts your skin’s delicate acid mantle. This can worsen inflammation and leave your skin parched and irritated. [6] Furthermore, widespread or long-term use of benzoyl peroxide, while effective for some, may contribute to bacterial resistance and can be excessively irritating for sensitive skin types, leading to redness and peeling. [7] As a result, this aggressive “killing” strategy can backfire, leaving the skin vulnerable to resistant bacterial strains or triggering new, reactive breakouts.
Product Pitfall #3: Acne Spot Treatments & DIY Remedies
The internet is absolutely flooded with “miracle” spot cures and do-it-yourself (DIY) remedies for acne. These range from applying teeth whitening paste to dabbing on lemon juice or even toothpaste.
But extreme caution is due when considering these unproven methods. Dr. Sandra Lee, widely known as Dr. Pimple Popper and a board-certified dermatologist, strongly warns that such ingredients can severely irritate the skin. They can promote post-inflammatory hyperpigmentation (dark spots) and scarring, and in some cases, even worsen acne by pushing bacteria deeper into the pore. [8] On the other hand, targeted, scientifically-backed treatments, such as products containing salicylic acid or prescription medications approved by a dermatologist, work gently and effectively to clear pores and manage acne without these harsh side effects.
The Good Bacteria Strategy: Restore, Don’t Erase
Emerging research in dermatology fundamentally shifts the focus from brute-force bacterial eradication to emphasizing microbial diversity and balance.
It’s increasingly clear that Cutibacterium acnes isn’t the sole enemy. Instead, it’s the specific unhealthy strains of this bacterium, and an overall imbalance in your skin’s diverse microbial community, that contribute to acne. A rich diversity of beneficial bacteria on the skin helps keep these “bad players” in check. [9, 10] For example, certain strains of Staphylococcus epidermidis, a common skin bacterium, have been found to actively suppress the growth of C. acnes and reduce inflammation. [11]
Future acne care is rapidly evolving. For instance, phage therapy, which uses beneficial viruses that specifically target and destroy harmful bacterial strains while preserving the good ones, is an exciting new frontier. Products incorporating this technology, like certain serums from brands such as Phyla, are already emerging. [12] As a result, the future of acne treatment may look more like careful “microbial gardening” than an indiscriminate war against all skin bacteria.
Dark Humor Moment
I once used lemon juice as a spot treatment for acne. I ended up preventing future breakouts… by literally burning a layer of skin off. Not exactly glowing results.
Why This Bacterial Perspective Matters
Traditional acne methods, which aim to kill indiscriminately, can inadvertently have several negative consequences. This approach can:
- Encourage resistant bacteria: By eliminating competing strains, you might create an environment where drug-resistant bacteria can thrive.
- Prolong the acne cycle: Damaging the skin barrier and disrupting natural balance can lead to persistent inflammation and recurring breakouts.
- Damage skin’s natural armor: A compromised skin barrier leaves your skin vulnerable to irritants and environmental stressors.
This explainer on How Bacteria on Your Skin Impacts Acne shows why understanding microbial imbalance helps you choose smarter, gentler methods. It highlights why some seemingly intuitive products can actually backfire, leading to prolonged skin issues.
Smarter Acne Care Steps
Ready to nurture your skin towards clarity? Here are some science-backed steps:
- Gentle Cleanse Twice Daily: Avoid over-washing or harsh, abrasive scrubs. Opt for a mild, pH-balanced cleanser morning and night.
- Swap Harsh Spot Treatments: Replace alcohol-based astringents with products containing salicylic acid or benzoyl peroxide (used sparingly and properly, under guidance if necessary).
- Preserve Your Skin Barrier: Always hydrate and moisturize your skin post-cleanse, even if it’s oily. Look for non-comedogenic products.
- Explore Pre/Postbiotics: Consider incorporating skincare products that support your skin’s microbiome, such as those with prebiotics (food for good bacteria) or postbiotics (beneficial byproducts of bacteria).
- Consult a Dermatologist: For persistent or severe acne, always consult a board-certified dermatologist. They can offer personalized advice, stronger prescription treatments, and guide you on emerging therapies like phage therapy.
Conclusion & Your Next Step
Acne isn’t your fault. And it’s certainly not simply about “dirt” on your skin. Instead, it’s a complex condition often rooted in microbial communities gone off balance. Aggressively killing all bacteria on your skin is an outdated and often counterproductive approach. Real, sustainable results come from understanding and restoring your skin’s natural harmony.
Your Next Step: Today, ditch any harsh scrubs and alcohol-based cleansers you might be using. Instead, commit to a gentle, balanced skincare routine for just two weeks. Track your breakouts, note any changes in skin sensitivity, and observe your overall skin tone. Watch how your skin responds to this kinder approach. Let your body’s feedback guide you to better, gentler products that support its natural ecosystem. Because clear skin isn’t about total bacterial wipeout . , . it’s about smart balance, quiet strength, and nurturing your skin’s own unique ecosystem.
Sources
- Journal of Investigative Dermatology. “Propionibacterium acnes, the resident skin bacterium, as a potential link between the environment and the immune response in acne vulgaris.” Published June 2013. https://www.jidonline.org/article/S0022-202X(15)35132-7/fulltext
- PLoS Pathogens. “The skin microbiota and its role in inflammatory skin disease.” Published November 2013. https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1003736
- Nature Scientific Reports. “A genomic analysis of the cutaneous bacterium Propionibacterium acnes in acne patients.” Published February 2014. https://www.nature.com/articles/srep03949
- UCLA Health. “Acne: New research on bacteria and treatments.” Published October 2, 2019. https://www.uclahealth.org/news/new-research-on-acne-bacteria-and-treatments
- American Academy of Dermatology Association (AAD). “Acne: Self-Care Tips.” Accessed July 17, 2025. https://www.aad.org/public/diseases/acne/skin-care/self-care-tips
- Journal of the American Academy of Dermatology. “Effects of various skin cleansers on skin barrier function.” Published January 2004. https://www.jaad.org/article/S0190-9622(03)02081-4/fulltext
- Dermatology and Therapy. “Benzoyl Peroxide for Acne: A Contemporary Review.” Published September 2017. https://link.springer.com/article/10.1007/s13555-017-0199-9
- Dr. Sandra Lee (Dr. Pimple Popper) Official Website. “Can You Use Toothpaste For Pimples? Dr. Lee Weighs In.” Accessed July 17, 2025. https://www.drpimplepopper.com/blog/can-you-use-toothpaste-pimples-dr-lee-weighs
- Journal of Clinical and Aesthetic Dermatology. “The Skin Microbiome and Its Implications for Skincare.” Published June 2020. https://jcadonline.com/skin-microbiome-skincare/
- Nature Reviews Microbiology. “The skin microbiome in acne vulgaris: lessons from next-generation sequencing.” Published February 2017. https://www.nature.com/articles/nrmicro.2016.155
- Science Translational Medicine. “A commensal bacterium of the human skin, Staphylococcus epidermidis, provides protection against Propionibacterium acnes-induced inflammation.” Published February 2015. https://www.science.org/doi/full/10.1126/scitranslmed.3010321
- Phyla Dermatology Official Website. (Information regarding their approach to phage therapy for acne). Accessed July 17, 2025. https://phyladermatology.com/pages/what-is-acne-phage-therapy